Key takeaways:
- The addition of hospital readmissions and ED visit measures increases the need for and accountability of home health agencies to improve patient outcomes.
- Improving outcomes can provide a competitive advantage to support growth
- Embracing digital technologies to support engagement between visits and patient driven outreach are critical to success.
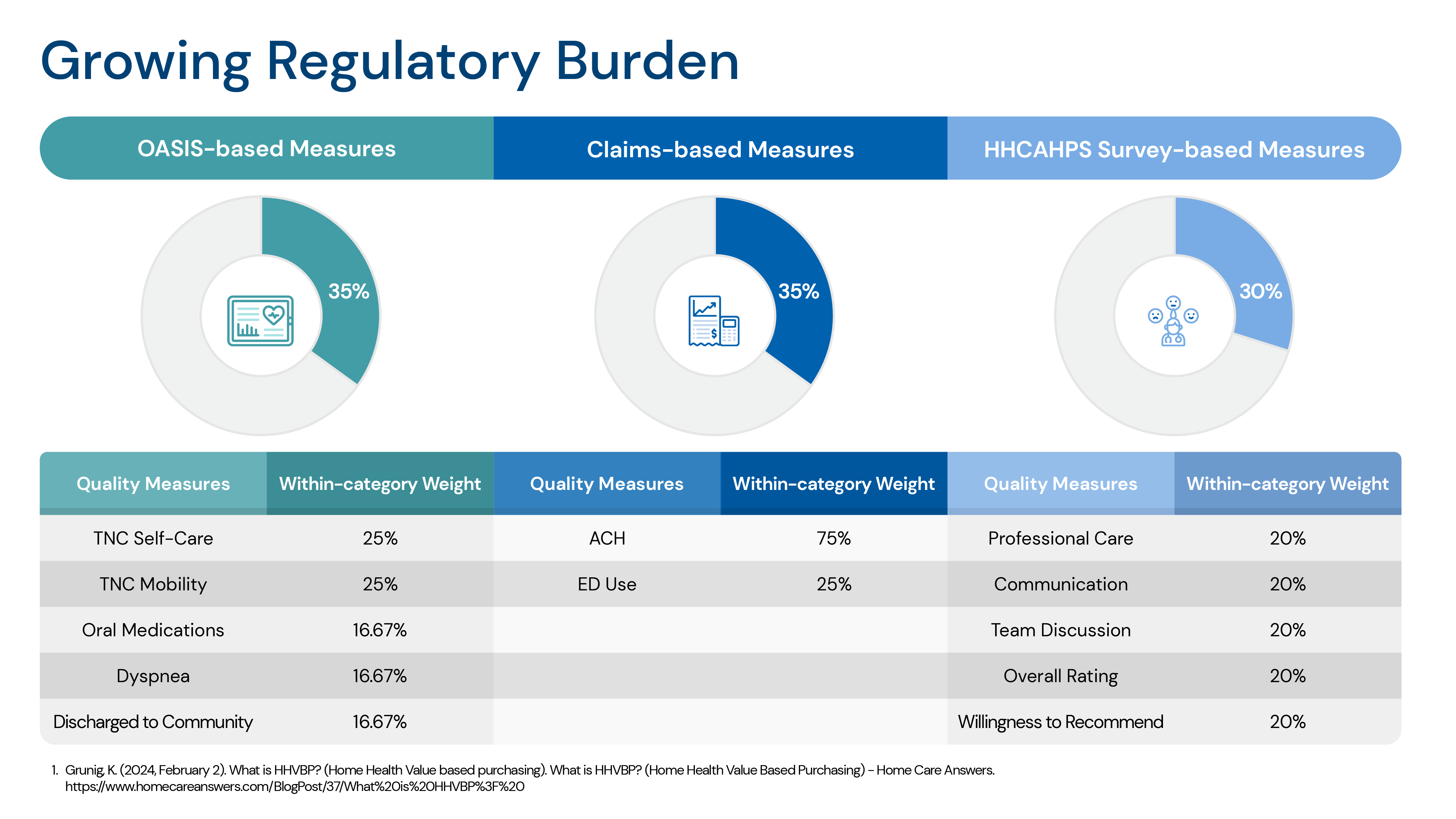
The Home Health Value-Based Purchasing (HHVBP) model is a payment model implemented by the Centers for Medicare & Medicaid Services (CMS). The program ties payment to performance on:
- Timely capture of Oasis data
- Avoiding hospitalizations and ED visits
- Delivering high patient satisfaction
Here are highlights of the HHVBP program on home health agencies:
- Increases emphasis on Quality: HHVBP encourages home health agencies to focus on improving the quality of care they provide to patients. Agencies must meet or exceed certain quality measures to receive full reimbursement and avoid penalties,
- Financial incentives and penalties: HHVBP introduces financial incentives for HHAs based on their performance on quality measures. Agencies that perform well may receive bonus payments of up to 5%, while those with lower performance may face penalties of up to 5%.
- Increased focus on outcomes and accountability: HVBP encourages a shift towards outcome-based care rather than volume-based care by adding claims-based measures focused on hospital readmissions and ED visits while they are under the care of the home health agency.
Agencies that consistently perform well under HHVBP may use their quality scores as a marketing tool to differentiate themselves in the marketplace and to support their growth strategies. Patients and caregivers can access home health performance scores through the Home Health Star Ratings website. Since most home health agencies have at least one other option for patients to choose from within their area, high-quality outcomes can be a competitive advantage in attracting patients.
Agencies who perform well and earn incentive payments can help offset the cost of technology investments and training they need to make to streamline operations, improve outcomes and patient experience.
Overall, HHVBP has the potential to drive positive changes in the home health industry by incentivizing quality improvement and promoting better patient outcomes. However, its effectiveness depends on the ability of home health agencies to adapt to the new payment model and effectively implement quality improvement strategies.
QliqSOFT can help. Our digital communication platform enables home health agencies to:
- Achieve operational efficiencies to do more with less
- Monitor patients between onsite visits and escalate those answers that indicate a need for agency contact
- Enable patients and caregivers to proactively reach out for guidance
- Increase staff and patient satisfaction


